
Cervical osteochondrosis is a progressive degenerative-dystrophic change of the intervertebral discs located between the first 7 vertebrae. Vertebrae 1-7 belong to the cervical spine.
Pathological changes occurring against the background of osteochondrosis lead to deformation of the vertebrae, which ultimately disrupts their blood supply, nerve conduction in the neck and innervation areas of damaged nerves.
Osteochondrosis of the cervical spine can be an independent disease, or it can be combined with osteochondrosis of other parts - thoracic and lumbar.
Main symptoms
The leading symptom of cervical osteochondrosis is pain, the localization and nature of which depends on the location of the lesion. It is most often felt in the neck-collar area, on one or both arms.
This disease is characterized by unilateral pain, and any part of the arm can hurt - the shoulder, the forearm, the hand and even the fingers. Many patients complain of headaches and dizziness.
The pain syndrome can also be felt in the chest, in the supraclavicular region, or spread to the back. For some, the pain is concentrated at the base of the neck or throat.
Osteochondrosis of the cervical spine is characterized by various symptoms and is often accompanied by impaired tactile sensitivity, muscle weakness, reduced visual acuity and hearing, rapid heartbeat and panic attacks.
Attention!
Sometimes osteochondrosis is complicated by vertebral artery syndrome, which may require urgent hospitalization of the patient.
First signs
In the early stages, the manifestations of osteochondrosis are more reminiscent of ordinary fatigue after a busy day and occur regularly. In the evening, there is discomfort and pain in the neck, heaviness and pain in the head, mainly in the occipital region. Cracking and creaking may occur when turning the head.
Signs of cervical osteochondrosis are more pronounced in women than in men and are often accompanied by an unstable psycho-emotional state. In addition, men suffer from this disease much less often.
Aggravation of chondrosis often occurs during menopause, when hormonal changes occur in the female body and the immune system weakens. During the diagnosis, certain difficulties arise due to the fact that the symptoms are similar to many other diseases.
Males are less responsive to little things like neck snapping and often simply don't notice suspicious symptoms. In addition, in men, the symptoms of cervical osteochondrosis may not appear for a long time, which is explained by the peculiarities of anatomy.
Men naturally have more developed and stronger muscles, which provide additional support to the spine. The muscular frame serves as a kind of armor that protects the vertebrae and prevents them from deforming.
Vertebral artery syndrome (VAS)
The clinical picture of SPA is usually represented by several symptoms, but only one of the possible ones can be observed:
- headache predominantly in the back of the head and at the base of the skull - basilar migraine, accompanied by classic symptoms: loss of coordination, nausea, vomiting, tinnitus, less often - speech disorder;
- dizziness that occurs when the head is turned. They may cause vomiting, darkening of the eyes and impairment of movement coordination;
- eye strain caused by stress, flashing spots and bright flashes in front of the eyes, and loss of visual fields in places. Patients may complain of pain, redness and feeling of sand in the eyeballs, inflammation of the conjunctiva;
- constant or episodic tinnitus, the nature of which varies depending on the position of the neck. There may be mild deafness, ear congestion and low sound unresponsiveness. In some cases, paracusia was detected - selective audibility of sounds, in which a person hears better in the presence of extraneous noise than in complete silence;
- Vegetative symptoms always appear during exacerbation of osteochondrosis and are most often combined with other symptoms. These may include hot flashes or chills, increased sweating, cold feet and hands, shortness of breath, increased blood pressure and poor sleep;
- TIA - transient ischemic attacks - accompany mechanical pinching of the vertebral artery and are manifested in double vision, temporary partial blindness, loss of visual fields, dizziness with vomiting, speech and swallowing disorders;
- Fainting can be the result of a sudden turn of the head or an uncomfortable position. The loss of consciousness is of variable duration and leaves weakness in the limbs;
- Drop seizures are sudden falls, usually without loss of consciousness, caused by a sudden rush of blood to the brain when the head is thrown back. The immediate cause is paralysis of the legs, but motor function is restored quite quickly.
Headache and dizziness
Most patients with cervical chondrosis have this symptom, but it may be absent. Dizziness is caused by compression of the main arteries and blood vessels, which interferes with the delivery of oxygen to the nerve tissue of the medulla oblongata and spinal cord.
As a result of mechanical trauma of the vertebral structures and chronic ischemia of the nerve fibers, the sensitivity of the nerve endings increases and irritation occurs, which ultimately causes cervical vertigo.
Dizziness can be accompanied by uncertainty of movements, an increase in heart rate, a jump in blood pressure, and increased sweating on the face and shoulders.
Headache is a frequent accompaniment of cervical chondrosis. Paroxysmal in nature, the duration of the attack ranges from several hours to several days. The intensity of the pain varies, but it occurs with enviable regularity.
The headache is caused by compression of the vertebral artery due to changes in the position of the vertebrae and discs. Due to the compression of the blood vessel, the blood supply to the brain is interrupted, which leads to pain.
Reference:
The cause of the pain can also be a muscle spasm characteristic of osteochondrosis.
Panic attacks
Panic attacks are also associated with a decrease in brain nutrition and cause the following symptoms:
- attacks of fever or chills, increase in body temperature;
- numbness, tingling in the limbs, muscle spasms, impaired motor skills;
- dizziness, loss of coordination, darkening of the eyes;
- pain behind the sternum or in the chest on the left side, rapid pulse, increased blood pressure;
- insomnia, fear of death or mental confusion, confusion;
- shortness of breath, difficulty breathing to the point of suffocation, lump in the throat;
- discomfort and pain in the abdomen, indigestion, frequent urination.
Sore throat
Osteochondrosis throat usually hurts when the 4th cervical vertebra is damaged or displaced. Localization is usually unilateral, as the vertebrae and discs are displaced to one side.
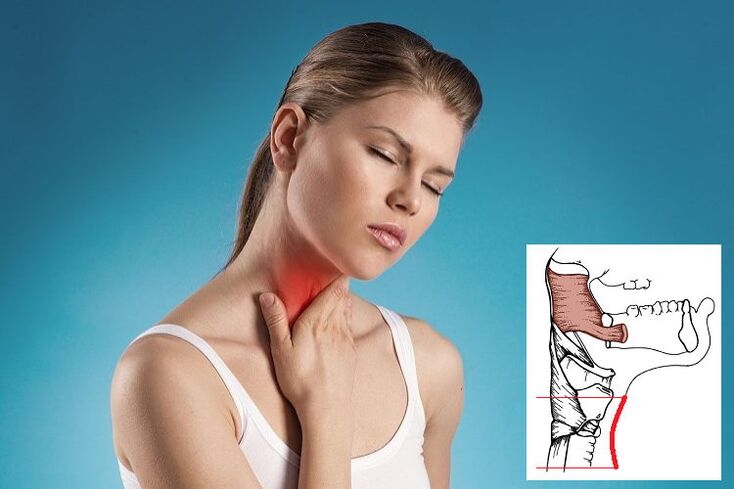
Due to pinching of the roots, spasm and tension of the pharyngeal muscles occur, accompanied by pain. The throat will feel heavy and full and it will be difficult to breathe. However, there are no mechanical obstacles to free breathing and swallowing, and there are no foreign objects or tumors in the esophagus and larynx.
It is typical that medicines against tonsillitis or sore throat, rinsing, inhalation do not have an effect.
The source of the pain is the area between the thyroid cartilage and the neck cavity. The nature of the pain ranges from mild to debilitating.
Treatment
The complex treatment of cervical osteochondrosis includes many methods - taking medicines, therapeutic exercises, physiotherapy and massage treatments. If desired, you can use folk remedies and prepare various compresses, infusions and decoctions.
In case of exacerbation of the disease, bed rest is recommended. Also, you need to lie on a flat and fairly hard, flexible surface - a sagging sofa or feather bed will not work.
Attention!
Severe pain requires immediate medical attention.
To fix the cervical spine, the doctor may prescribe wearing a Shants collar. It supports the neck in an anatomically correct position, eliminating movement and thus pain.
Medicines are selected based on existing symptoms and diagnostic results. If hernias and protrusions are detected, the treatment may be surgical.
| Drug | Action |
|---|---|
| Vasodilators and nootropics | Improves cerebral circulation, dilates blood vessels, relaxes smooth muscles, reduces the frequency of nerve signals |
| Preparations containing chondroitin and glucosamine | Restoration of the cartilage tissue of the discs, slowing down the degenerative processes |
| Muscle relaxants | Alleviation of muscle spasms |
| Nonsteroidal anti-inflammatory drugs | Alleviation of the inflammatory process, tissue swelling |
| Pain relievers | Pain relief |
| Opioids | For severe pain that cannot be alleviated with traditional methods |
| Vitamin complexes containing vitamins B, A, C and calcium | Nerve, muscle and bone tissue strengthening, general healing effect |
| Antidepressants and sedatives | Coping with the stress of constant pain |
Treatment at home
It is not recommended to lie at home and follow bed rest for too long, and after the acute symptoms subside, it is necessary to switch to active actions. You should start with simple exercises and gradually move to more intense exercises.
- Exercise 1 - self-extension. Stand down with your arms along your body, tilt your head to the right and simultaneously reach down with your left hand. Stay in this position and repeat the exercise on the other side.
- Exercise 2 – self-massage. Place the towel on your shoulders and pull it in one direction or another by holding the edges.
- Exercise 3 – turning the head left and right, tilting to the right and then to the left shoulder.
- Exercise 4 – same as hand counter: press on your temple while turning or tilting, creating additional resistance.
Tips for preventing osteochondrosis
Tip #1
Physical education is the main way to fight the aging of the body and the development of intervertebral disc dystrophy. Daily exercise and a visit to the pool at least once a week are usually sufficient. All this makes it possible to strengthen the muscular ligament of the spine.
Tip #2
Even a healthy person needs a massage, they are recommended to be done annually.
Tip #3
It is very important to monitor your weight and avoid gaining extra pounds.
Tip #4
If you work in a forced position for a long time, you should take a break, change your body position, and warm up.
Tip 5
Proper nutrition means consuming sufficient amounts of vitamins and microelements with food.
Tip 6
Try not to lift or carry heavy objects, and if you must, wear a support brace.
F. A. Q
When should you see a doctor urgently?
The reasons for an immediate consultation and even an ambulance call are as follows:
- persistent numbness in the arms or legs;
- severe pain that is not relieved by conventional pain relievers;
- movement disorder;
- severe headache, dizziness, loss of coordination and other signs of a cerebrovascular accident;
- the "stuckness" of the back in a certain position sharply restricts movements.
Is it possible to cure chondrosis forever?
No, it is a chronic disease with periodic exacerbations. Even after treatment and following all the doctor's recommendations, the cartilage in the affected area of the disc is replaced by scar tissue. That is, the structure of the segment has already been damaged, and this process is irreversible. However, with certain efforts of the patient, a high quality of life can be achieved.



















